Des del campus
7. From campus
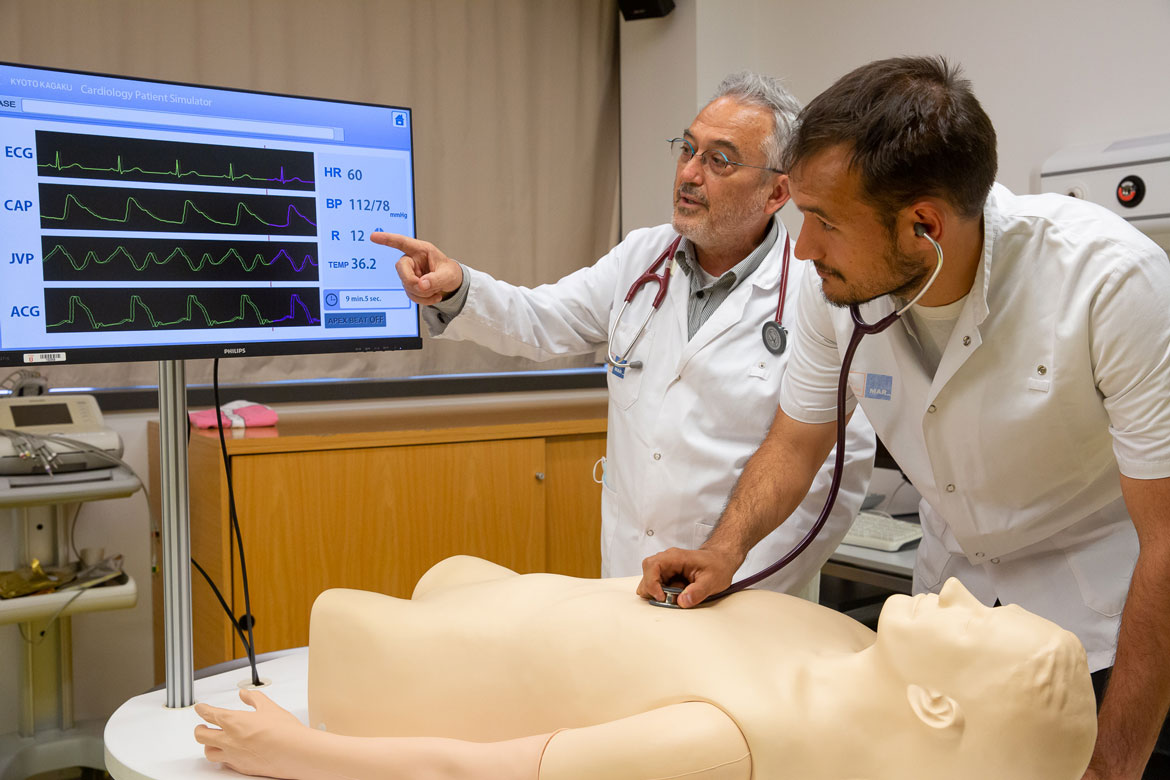
An introduction to the healthcare reality through clinical simulation
Clinical simulation is a learning method in which the student has to solve a clinical case in conditions as similar as possible to real life. When the methodology is applied correctly, it enables an active, individualized, reflective learning, adapted the student’s needs and to different clinical situations. Moreover, it does all this in a safe environment for both the patient and the student.
In the mid-twentieth century, most plane crashes were caused by human error. One thing that has helped to improve this situation is flight simulators, which were first used in the late 1920s, and, beginning in the 1980s, became increasingly realistic. Today, simulation is an essential part of pilot training, allowing pilots to practice what to do when faced with complications that could arise during a flight without actual risk.
Meanwhile, the manikins are gradually becoming more and more realistic: they simulate physiological and pathological conditions and make it possible to replicate numerous clinical scenarios.
In the health sciences, simulation was first used in 1911, at Hartford Hospital, in Connecticut (USA). It took the form of life-sized manikins used by nursing professionals to practice skills such as dressing and mobilizing patients. But it was not until the 1960s that the prestigious Viennese anaesthesiologist Peter Safar asked a toy manufacturer to create a manikin for the purpose of practising complex skills, such as cardiopulmonary resuscitation (CPR). In the 1990s, manikin simulations began to be enriched with constantly evolving technological advances. At first, simulation was used in specialities that often treat critical patients, such as intensivists, since in these environments, practice with certain techniques has a major impact on patient survival. It was subsequently implemented with professionals and postgraduate students, and more recently it has begun to be incorporated into undergraduate training. Meanwhile, the manikins are gradually becoming more and more realistic: they simulate physiological and pathological conditions and make it possible to replicate numerous clinical scenarios.

‘Specifically, in the bachelor’s programme in Medicine, simulation is already part of the course plan for eleven subjects: Patient-Doctor Relations, Specific Pathophysiology, Nutrition, Foundations of Surgery, Locomotive System, Otorhinolaryngology, Integrated Internship in Medical-Surgical Pathology I and II, Rotating Internship, Gynaecology and Psychiatry’, explained Meritxell Girvent, the clinical simulation coordinator at the Faculty of Health and Life Sciences. Next year, they will probably be incorporated into new subjects, such as Paediatrics and Cardiology.
Key stages of the methodology
The methodology used in clinical simulation has also evolved in recent years and consists of several stages. First, the lecturers look for a case and adapt it to the objectives they wish to achieve with the simulation, depending on the subject and student skill level. They then prepare the case, including the diagnostic tests that can be provided to the students when they are solving it. There is always a facilitating lecturer on hand with expertise in the methodology, as well as a lecturer specialized in the subject matter of the case being worked on in the simulation.

At the start of the simulation, the people involved introduce themselves and an ice-breaking dynamic is done. According to Girvent, ‘The aim is to create a framework of trust, so that the student clearly understands that he or she is in a training and learning environment. On the one hand, the simulation will serve to consolidate everything they do well; on the other, it does not matter if they make a mistake; on the contrary, it is a learning opportunity.’ To achieve this, several basic principles need to be taken into account. ‘We start with the premise that everyone doing the simulation with us is intelligent, is striving to do their job as best they can and wants to improve. Respect is also key. When someone disagrees with another person’s decision, the issue is always approached with arguments and by trying to understand the other person’s mindset. So, we do not judge mistakes: we turn them into reasons to learn. The goal is for the students to leave the simulation with more knowledge and understanding than they had coming in’, she stressed.
‘The aim is to create a framework of trust, so that the student clearly understands that he or she is in a training and learning environment. On the one hand, the simulation will serve to consolidate everything they do well; on the other, it does not matter if they make a mistake; on the contrary, it is a learning opportunity.’
Another principle is the confidentiality of the case, so as not to condition students from other groups before it is their turn. Everything said or done in the simulation must also be kept confidential. Additionally, there is a willing suspension of disbelief, wherein the teachers do their best to make the environment as realistic as possible and students are asked to make an effort to believe they are in a real-life setting.

Once the students are in the scenario, a high-fidelity manikin or actor is used to simulate the patient. At the same time, the environment is adapted to be as realistic as possible. ‘At the Mar University Campus, clinical simulations are done in shared classrooms. We have a doctor’s office classroom and a classroom that can be adapted to resemble a hospital room, an emergency room cubicle, an operating theatre, a delivery room, an ICU room, an emergency cubicle at an urgent care facility, etc.’, Girvent explained. Some of the specific cases students encounter in the simulations are acute myocardial infarctions (heart attacks), gastrointestinal bleeding, polytrauma caused by a motorcycle accident, or a pregnant woman with preeclampsia. There are also cases of patients who have come in because they are experiencing dizziness, fever or acute abdominal pain. The simulations further allow participants to learn how to talk about sexually transmitted diseases or treat a patient experiencing a psychotic episode or major depression in an emergency setting.

Some of the students do the simulation whilst the rest of the group watches them live from an adjoining classroom. The observing students take notes on all the things they would do the same or differently to help them reflect and work on the material during the debriefing, which is the final stage of the simulation. When the participants ask for the results of the tests that they would order, these results are also provided to the classmates watching the simulation. ‘If at any point the participants consider it appropriate to consult someone with more expertise, they always have support. They can contact a specialist – who is in the control room – by phone and ask them any questions they might have, just as they would in a real-life clinical setting’, Girvent explained.
The teachers’ role is to support the students in this process so that they can draw their own conclusions and learnings through inquiry and reflection based on an objective fact observed during the simulation itself.
Once the simulation scenario is over, the last stage, or debriefing, begins. This stage consists of a more emotional first part, in which the students are asked how they feel and how they think the case went. This is followed by an analysis and reflection stage, which is not intended to judge the students’ behaviour, but to understand the criteria that guided their decisions to act in one way as opposed to another. The teachers’ role is to support the students in this process so that they can draw their own conclusions and learnings through inquiry and reflection based on an objective fact observed during the simulation itself. Finally, the session concludes with a summary and with each person sharing their main takeaways.
Learning together to work together
In other subjects, students do interprofessional simulations. ‘In the 2014-2015 academic year, a group of teachers from the different health science schools at the Mar Health Park – the Bonanova Institute of Vocational Training in Healthcare, the Mar Nursing School (ESIMar), and the Mar Campus University Teaching Unit from the UPF-UAB bachelor’s degree in Medicine – came up with the idea of pooling our knowledge to offer innovative training. To this end, we launched a clinical simulation activity in the teaching field, with the peculiarity that it would be of a multi-professional character and spirit’, explained Lluís Molina, one of the drivers of the initiative and the first lecturer to include interprofessional simulations in the subjects he coordinates.
This initiative, called ‘Learning together to work together’, sought to conduct the most realistic simulations possible with students from different disciplines who would go on to work together in the field of healthcare: assistants, nurses and doctors. ‘The pilot test was a success; it was very well received by our students. Encouraged by these results, in 2016, we implemented this activity in a structured way in the teaching for the bachelor’s degree programme in Medicine’, he added.
‘In 2018, we inaugurated the current simulation room facilities, equipped with all the necessary technology and tools to fully carry out this teaching activity, which we consider quite necessary. We have grown, we have increased the teaching staff and we also have dedicated technicians for this activity, who are an essential part of the project’, Molina explained.
Learning technical skills
‘The simulations in which students have to solve a clinical case follow a complex methodology with clearly defined stages. However, we also do other types of simulations on campus in the clinical skills classroom to practice more technical procedures’, said Girvent. The classroom has several highly realistic manikins, allowing students to learn and practice different techniques, such as suturing or CPR. There are also models for practicing prostate, genital, breast and eye examinations, etc. The material the manikins are made out of has also evolved a lot, and they can be adapted to more and more situations, making it possible for students to explore different diseases. A good example is the cardiovascular system manikin, which allows them to learn to auscultate and differentiate between the various sounds of the heart tones and associate them with different diseases. There is a similar manikin for learning to do respiratory system examinations and distinguish the different pathological noises.
‘Simulation already plays an important role in medical education today. This role will gradually become more important as virtual reality techniques are incorporated as well. Simulation is still relatively underdeveloped in our country; but we are aware that it is an unavoidable part of healthcare studies. In fact, the faculty could play an important role in creating a benchmark centre for our environment. We are already familiar with the best simulation centres in Spain. In the coming months, we will visit the ones considered international benchmarks, to learn about their organizational and technical details and facilitate the implementation of this field of learning at our faculty’, explained Joaquim Gea, dean of the Faculty of Health and Life Sciences at UPF.
‘Simulation already plays an important role in medical education today. This role will gradually become more important as virtual reality techniques are incorporated as well.
According to Girvent, ‘When students do their internships, it is crucial for them to see how people work in a real-life clinical environment; nevertheless, they play a more passive role, strongly based on observation, which is very important. Clinical simulations allow them to take responsibility for the patients, as they have to make decisions.’ Another very important benefit of simulation is that it can be used to work on a wide range of cases. ‘For example, not all students will encounter the acute phase of a heart attack in their internships. With these tools, we can choose first-line objectives and frequent cases, in order to work on key aspects of the subject matter. In fact, in a seminar with a single manikin, we can sometimes simulate all the diseases we need’, she added.

This methodology complements the training received in the classes and internships. ‘Until a few years ago, the technical skills needed to deal with clinical cases were acquired through clinical practice. However, the regulations are increasingly focused on ensuring patient safety, which is why these tools need to be well-integrated into the course plan. We are expanding the subjects that include simulation; new cases are being added to ensure constant evolution’, she stressed.
According to Molina, ‘Our challenge now is to continue this growth, in terms both of expanding and of the teaching staff involved in this teaching methodology. I would add that it is an inevitable path requiring constant maintenance. One need only look to the major renovation of all the material in the skills classrooms done this academic year.’

‘In my view, simulation greatly increases students’ motivation to learn, and they respond very positively. In the surveys we do about simulation, the participating students rate it very highly as a learning tool and say they would like to use it more’, Girvent concluded.
‘Until a few years ago, the technical skills needed to deal with clinical cases were acquired through clinical practice. However, the regulations are increasingly focused on ensuring patient safety, which is why these tools need to be well-integrated into the course plan’
According to José Canela, a sixth-year medical student, ‘Simulation has given me the opportunity to test myself in extreme situations, which I will be able to expose myself to in the future with the peace of mind of knowing no one will be harmed. The immersion is much more thorough than it might at first seem, allowing you to put your knowledge into practice and become aware of your strengths and weaknesses in a much more life-like situation than a multiple-choice test or written exam.’ ‘Nor is it the same as being in an internship,’ he added, ‘where a professional might take your place or correct you if you make a big mistake: it is just you and you are responsible. To me, it seems like a very stimulating, but also very effective way to learn. Plus, it is unlikely to become monotonous for students.’
According to Roger Conesa, another sixth-year student, ‘Simulation is an ideal way to fully integrate knowledge through practice. It especially drives home the things you need to improve so you don’t forget the next time, whilst also helping you internalize and consolidate the things you have done well so you can maintain them, all with the confidence that comes from knowing it is an ideal learning environment.’